 |
| Heather in Hawaii around 2009, maybe? |
My sister —my beautiful, baby sister — died on January 28 this year.
I've been wondering how or if I would ever write about it anywhere publicly for a while now. I've posted bits and pieces about what I went through on Facebook, a tiny bit on Twitter, some of it in my journal, but mostly I've just thought about it over and over, speaking with the others who went through it with me, like my mom, other family members, and some of Heather's friends. In order to keep some semblance of privacy I've tried not to use any names, but when I say "we," I usually mean me and Heather's friends or some of our family, or sometimes Heather and I. Also, I have decided not to write about any of Heather's specific health issues to honor her privacy.
Anyway, it's just all too big; the memories and feelings take up huge bits of real estate in my head and heart. So, this is my attempt to write about what happened and what I am going through now. It's a long read. If you don't feel like going through it all, you can skip to the end to see links to her obituary.
What Happened
When Heather first went into the hospital in mid-December, we knew it was serious, but we also thought it was survivable. My sister was a very private person, so at first we didn't even know she was in the hospital, until her best friend, the one who had called 911 and got her there, got her permission to let me and our mom know.
Christmas was one of my sister's favorite times of the year. Mine and my mom's as well. We always tried to make it special for each other. But this last season, it felt rushed and off, and that was before she ended up in the hospital. It was almost as if Heather knew she didn't have much time. She got her Christmas gifts out to us fairly early. And we tried to get ours to her early, but not early enough, it turned out. I now think of it as the Christmas-that-wasn't.
By Boxing Day, the hospital let us know that Heather's condition was not, after all, survivable, except by a very slim margin, or a miracle. She had asked for help in getting her affairs in order. I had been the emergency contact with the doctors because my mom has some other health issues that made it difficult for her. But, I didn't have what I needed to get to Oakland, and my sister didn't have the wherewithal to access her own funds to help. I was going to go by train because that was doable, when I got a call that it would be best if I could get there sooner rather than later. I had a small amount left of my IRA funds that I had slowly been eating away at since I haven't been able to find work. So, I used up some of the last of that fund to get a ticket, but you know that doesn't happen quickly. It always takes a few days. And by the time it all "settled" I ended up getting a ticket that was overpriced, but got me there, in Oakland, by the evening of January 2. By then, the doctors were sure that Heather would be gone in the next few days.
As soon as I landed, I went straight to the hospital. It was night, I was exhausted and scared. In the two-three weeks that my sister had been in the hospital, we hadn't really been able to communicate with her very well. The toxins in her system had messed with her head (sometimes she would even pull the tubes or IV lines out, or try to anyway). Her phone was either in a locked cabinet or out of juice. Sometimes, occasionally, we'd get a nurse who would make time so we could talk to her on the phone or via a tablet or iPad. But these were just moments of jumbled conversation. Cards that my mom and I sent to Heather were never given to her, just stuffed in with her clothes and locked in a cabinet. I didn't even see them until after I went through her clothes when she was transferred to hospice. There were no Christmas trees or cards or decorations or anything to celebrate. I wanted to burst into her hospital room and try to do something about it! I wanted my baby sister to at least have some kind of celebration in her life.
And of course, when I tried to do that the next day, first thing she said to me was, "don't do that to me."
It was so sad.
But, back to that first evening.
If you've been in hospitals recently, you know what it's like. There's security, limited number of visitors per patient (unless they're under palliative care and then that number is loosened up a bit), none of the vending machines work, and if there are coffee shops or cafeterias, they're all closed by like 2 or 3 p.m. And I'm not sure why, but at the time, Highland Hospital never seemed to have any orange juice. Every time she asked for orange juice she got apple juice. Once it was cranberry. It got to where she just wouldn't touch it when it came. So we started bringing in OJ for her. We were told it was better if she ate, so we wanted to make sure she ate something. Plus, she was dying, for pete's sake! The least we could do was make sure she had the orange juice she loved and craved.
Hospitals, for all that they're there to stabilize and get people on the road to healing, are not user friendly.
Anyway, that first evening, there I was, juggling my cane and my luggage, walking hallways that seemed to go on forever (after a day in the airport that had seemed to go on forever) on two knees with osteoarthritis, a bum left ankle, a right foot with its own issues (plus a handful of other health issues I am dealing with) to finally get to my sister's room. It was the same walk I took almost every day, more or less, for the next two weeks as we figured out how to settle Heather's affairs and what her next steps were.
Those long hallways, standing in line at security, walking even longer hallways to the elevators and up to Heather's room, with me hauling in photos and food and my laptop and her iPhone, etc., still pop into my head at the most unexpected times. Day after day, and not always to the same room, I wondered how I would I find her. What condition would she be in? Because, of course, as Heather's condition changed, her room changed. Don't know why they couldn't just leave her in the same room, but every few days, as soon as we got used to how to get to her, sure as anything, she'd be in a new room.
The doctors had expected Heather to be gone (and by gone, I mean dead) by the 5th at the latest, and I was crossing my fingers for her to be with us until at least the 9th, so we could "get things done." Each day she had maybe an hour or two when she was at her most coherent, snatched at small intervals. That decreased over time, eventually, and it was time we needed for her to be able to make decisions and let us know what she wanted with the Will, with hospice, with saying goodbye to friends and family. It was hard; hard on her and hard for us, her friends and family, who were with her. She wanted to sign blank checks so I could access her accounts for making some of the arrangements, but her hands wouldn't work. When it came to her Will, we needed to use a traveling notary ($237) who would verify she was cognizant and who used a thumbprint to show her intention even if her signature was unrecognizable. One of the days when she was the most aware and we were discussing it, I captured her in a video as she stated very articulately what she wanted done. She was exhausted with the effort it took at the end of these days. It was so hard to watch. However, we were able to get a Will done and signed and witnessed by the 7th, thankfully.
The palliative care team, which really did a very good job of watching over Heather's care in the hospital, had said it was okay for me to spend the night with her (comfort care rules), which I tried to do. But some night nurse always chased me out, even when Heather said, very clearly, that she wanted me to stay there (and it wasn't like I was in the way, I was just sitting in a corner of the room), and even when we told the nurses that the palliative care doctor said it was okay, they wouldn't listen and would make me leave. I really begrudged that time with her. I wanted to stay with my baby sister and spend as much time with her as I could. Each night when I went home, when her friends left, we didn't know if that would be last time we saw her alive. Whenever I received a phone call with an Oakland area code, I didn't know if it might be the hospital letting me know if it was time. Had she died? So, I really wanted to stay each night and wanted to put up a fight about it, but I also needed the nurses and doctors to be on my side, Heather's side, our side, for helping us to make the right moves. So, I went home, or back to Heather's home, actually, and spent the evenings wondering how she was, regretting not seeing her more, bawling over the loss (I had almost fallen into tears in Heather's hospital room when I first got there, but her head whipped around and she flat out ordered me, "Don't cry!" So, I set myself the task of holding back any crying until I could get safely back to her place). I was also going through her things, deciding what could be thrown away and what would need to be packed away eventually. (Tossing out the old food was easy. But it was when it finally hit me that she would never be coming back to her place and I started throwing away her underthings and socks that it broke something inside me.) Then each morning I'd get back up, wondering how Heather had fared over night, and start the whole process all over again.
It wasn't all grim. There was some humor. When I was in her apartment I found four (4) copies of her apartment key. When I asked her why she had so many she gave me a wide grin and said, "I'm paranoid!" It was a funny moment.
At first, it was all crisis mode. Then, after the emergencies were seen to, such as medical decisions and getting the Will signed, we had to make the other decisions, such as what measures, if any, Heather wanted the hospital to take to keep her alive. The "Do Not Resuscitate" order on her chart was her decision. I was there and holding her hand when we talked about it. She was not alone.
Finding a Hospice
Then there was the matter of hospice or comfort care: hospital, home, or hospice? Believe it or not, but the Bay Area doesn't have that many actual hospices. A lot of "hospices" are just wings of nursing homes or rehab facilities, and most of them are full up, so you have to get on a waiting list. They (doctors and providers and insurance companies) usually depend on people spending "hospice" at home, which means the family provides the care with an occasional medical technician coming in to make sure they're doing things correctly. And this might be fine if the home is a ranch-style single-family home on one level with several bedrooms and enough family members to pitch in with care, but not such an easy set up if you live in a 300-square-foot studio apartment with a hinky plumbing system that's got a steep driveway and two sets of stairs to get to the front door and is out in the middle of the Oakland Hills in the midst of winding roads (very pretty, but not so practical), with no street lighting, no public transportation, and hardly any parking. Oh, and it was going to be me being her caretaker, and maybe a couple of friends who could make it when they could.
But then, at first the doctors assumed Heather wouldn't even make it to hospice, that she would die in the hospital, which is why she was changed to a system called "comfort care," which means taking away the machines, adjusting medications so it's more for keeping the patient comfortable, and allowing more family to visit. However, Heather was strong and dying on her own schedule, which was not as quickly as the doctors at the hospital thought. So we were being gently pushed to get her transferred. There was a waiting list for the few hospices in the Oakland area (Alameda County), and again, while one social worker tried to push for us to take her home, there was no way we were going to be able to do hospice at Heather's studio apartment.
 |
| Heather and a friend. |
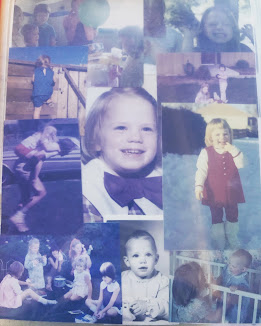 |
| Photos of Heather |
 |
| Heather and Mom one Christmas. |
 |
| Mom and Heather at Mom's 80th birthday dinner. |
 |
| Our cousin, Heather, me, and Mom. |
 |
| Heather and I in about 1979. |
In the middle of all this, when Heather was able, we were trying to phone or Facetime friends and family. Our stepmother had brought in some photos of Dad and Heather and I when times were better. In going through Heather's apartment I found other photos that I brought in for Heather to look at when she was aware. They were photos of her with friends and family, or from some of her travels to Cuba, Puerto Rico, Italy, etc. Some family members were able to schedule visits. We were going to make sure that Heather could feel the love of her friends and family around her. I kind of failed at this, though, as sometimes people would call or text Heather and I would be so distracted with other things that she wouldn't get the messages until later. But we were trying.
Mission House Woodside
The hospital social worker had overheard us talking about friends and family who lived on the peninsula in San Mateo County. It was after the 9th and I initially thought I would be going home by the 10th. But Heather was still around, albeit with a DNR wrist band and sleeping more and more each day. I decided I needed to stay for the duration, whatever that needed to be. Both the hospital and her insurance wanted her transferred elsewhere, and I've already pointed out some of the issues we had with those various "elsewheres." However, there was a hospice the social worker knew about on the peninsula, Mission Hospice Woodside in Redwood City, which did have a bed open. I am so glad we went there. It was further away from her apartment than the hospital (an hour's drive via Lyft or Uber instead of the 20 minute drive to Highland Hospital), but it was exactly the place she needed to be.
The day we transferred to the hospice was Friday, January 13 — Friday the 13th. Heather and I laughed about that. I was able to ride in the ambulance with her when they transported her there. We didn't talk much, though, just held hands. It was a bumpy ride and we were both pretty nervous.
What I remember most about Heather getting settled is the kindness of the staff as we were going through the steps of checking her in, and the moment when we got into the room and the nurses were setting things up, surrounding Heather. They asked me to step out while the settled her, but she was nervous and scared and suddenly more aware and looked up and around and saw me. Her eyes were wide. I said, "I'm here. I'm right here and I'll be right back as soon as they're done." She nodded and I stepped out. I was scared and nervous, too.
Now, here's something I learned that is crucial in anyone's understanding of a hospice. While a hospital is there to stabilize and get the patient onto the road to recovery, a hospice is there to help provide comfort to someone who is most likely in their final days. While a hospital will also try to keep a patient comfortable, that's not their primary goal. And while the medical professionals do see a lot of death, they don't specialize in what people go through at the end of their lives. So, for example, one of the differences was that the hospital brought in meals on a regular schedule. While the hospital pared down the meals because Heather didn't eat very much unless we helped her, they still kept up that schedule. At the hospice, however, as it was explained to me by the administrator when we checked in, there was no set schedule. If a client (not patient, since hospices are not considered medical facilities the way hospitals are) was hungry, they could ask for a meal, and meals were made on site. And they even had orange juice! Heather's first and only meal at the hospice was orange juice and tomato soup, both very tasty. However, 20 minutes later Heather was in pain and needed pain medication.
Back in the hospital we hadn't connected Heather's eating with her pain. And if the staff were aware of how it was all processing, they didn't explain it to us. However, one of the nurses at the hospice explained to us that with the nature of Heather's illness, her body had problems processing food, which resulted in pain about 20 minutes after she ate. And as time went on and her system broke down more, it would have more problems processing food, and create more pain. One of the best ways to navigate that, the nurse pointed out, was to make sure that Heather had just enough to satiate the need for something in her mouth, such as sucking on ice chips or using oral care swabs, and limit any food intake, and thus prevent, as much as possible, any onset of pain.
The End
So, that is what we did, helping relieve Heather's dry mouth with oral swabs, water, and ice chips. Over the course of the next couple of weeks, her friends, our stepmom, and I took turns hanging out with her at the hospice, trading off spending the night with her, reading to her, watching some of her favorite cop and western shows as we had in the hospital. More family came to visit. Mom called and talked to her. She wasn't usually responsive, partly because of the pain killers, but we wanted to make sure that if there was any awareness, she'd know she was loved.
The staff took excellent care of her, always making sure she was as comfortable as possible and always treating her with great kindness and respect. In fact, when Heather had first gone into the hospital, her best friend's wife had given her a bracelet to wear that had a Tibetan prayer inscribed on it. She always wore it. When she went into hospice, one of the nurses, who was from Nepal, recognized the prayer and prayed it with her one day during his shift. It was so kind.
Heather passed over late on the evening/early morning of January 27/28. Her best friend was with her at the time. She was with someone who loved her and I will always be grateful for that.
After she passed, while we were waiting for the crematorium to pick up
her body, the staff did what they called a rose petal ceremony where her
body was wiped down with lavender oil and water, she was dressed in
regular clothes, and then her body was sprinkled with rose petals. And
then we sat with her while we waited. This was my baby sister. I remembered holding her when she was a baby and first came home from the hospital when I was three years old. Since then, we had played and fought, been best friends, and not talked to each other. Whenever I thought about growing old, it was with my sister by my side. That night, it was difficult for me to grasp that her spirit was no longer in her body, that I would never see her again, that she wouldn't just wake up and tell me to get over myself.
 |
| When we said goodbye to Heather in Half Moon Bay |
Aftermath
It has been five months since then, but sometimes it feels like it's been a year, sometimes it feels like it just happened last week. I had gone up to Oakland for what I thought would be a week and ended up staying for a month, and it felt like a year. As they say on Doctor Who, time was all wibbly-wobbly — is still all wibbly-wobbly. While everywhere else it was becoming spring and summer, and the rest of the world was talking about Mother's Day, and then graduations, and then Father's Day, I was feeling like it was still winter, like in Narnia — always winter, never Christmas.
We scattered Heather's ashes in Half Moon Bay at the end of April. It was where we had scattered our dad's ashes; she had requested it especially. It was a perfect day and all the right people were there. Still, it's been a hard 2023 for everyone who knew Heather and loved her. I can only write about it from my own perspective, but I know I'm not the only one who mourns her loss and misses her terribly. Her friends and other family members all have experienced, or are experiencing, their grief in just as many different ways. She was an intelligent, beautiful, and vibrant person and she will always be missed.
If you never met my sister and would like to read a little bit more about her, you can find links to her obituary below. The one in the Bellingham Herald even has a short video with photos.
Heather's obituary in the San Francisco Chronicle: https://www.legacy.com/us/obituaries/sfgate/name/heather-olivier-obituary?id=43548527
Heather's obituary in the Bellingham Herald, which has a short video: https://www.legacy.com/us/obituaries/bellinghamherald/name/heather-olivier-obituary?id=42840719
